"I know you can't live on hope alone; but without hope, life is not worth living. So you, and you and you: you got to give them hope; you got to give them hope."
—Harvey Milk
—Harvey Milk
HOPE ALLIANCE (Treatment Access)
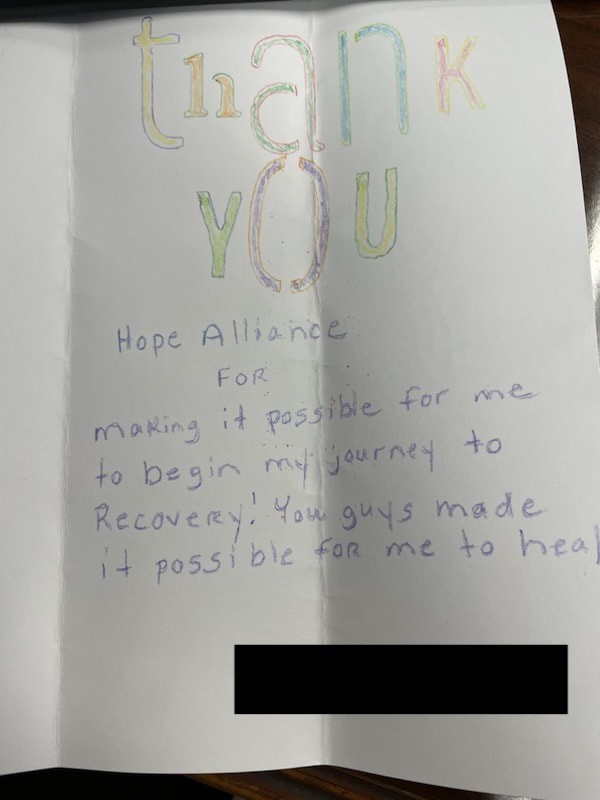
Hope Alliance (HA) is funded and sustained by grants only and heavily relies on its partners for the work they do. HA offers treatment access to anyone seeking help to overcome addiction. Recognizing that addiction is a disease and that law enforcement cannot arrest their way out of this epidemic, the Wilson Police Department (WPD) partnered with the Wilson County Substance Prevention Coalition (WCSPC) to create Hope Alliance. Hope Alliance partners with many detox facilities and treatment centers in North Carolina and surrounding states to get individuals the help they need. The process really is as simple as making the phone call or dropping by the WPD and having an assessment done.
Hope Alliance is housed at the Wilson Police Department. WPD does all of the hands-on work under the coalition umbrella with only one staff member, the HA Coordinator, who depends on community partners to assist with funding and treatment referrals.
When the discussion of creating treatment access for individuals arrested on drug charges arose, a group of stakeholders came up with the name Hope Alliance because hope is defined as “the desire accompanied by expectation of or belief in fulfillment, a confident expectation” and the word, hope, is associated with many recovery groups.
The current vision of HA is for the individuals they serve to have access to more affordable quality treatment and more financial resources to send clients to treatment.
Anybody can access treatment via HA, just call or walk in off the street. Individuals can also be referred to HA by lawyers, doctors, and other professionals.
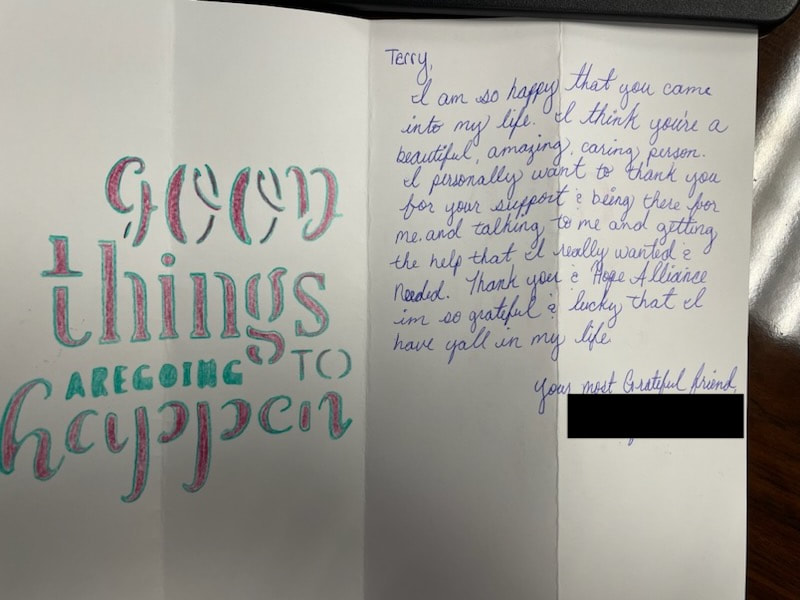
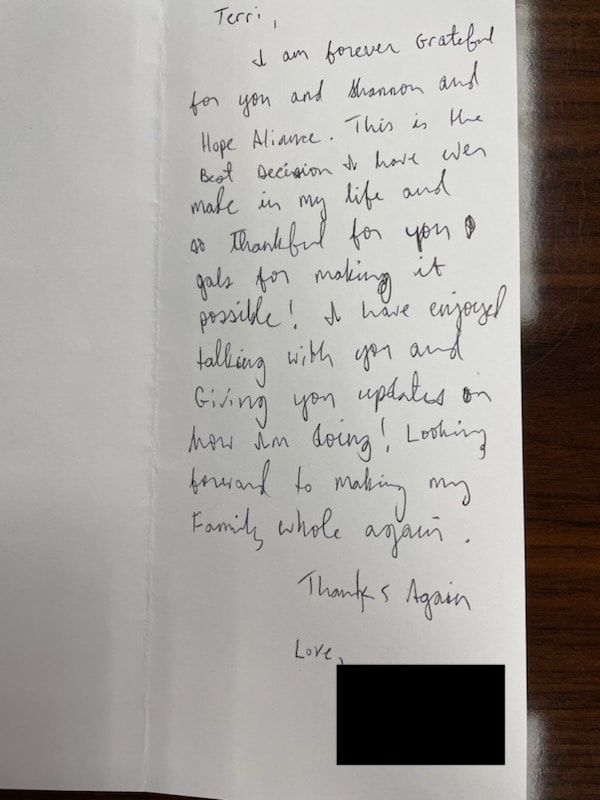
Mrs. Shannon Nichols, former HA coordinator, has had many success stories during the five years in which she has worked for HA. One time, after a big press conference and story The Wilson Times did about HA, a client with an old sports injury came in. He said that he had been prescribed a narcotic when he was first injured and eventually became addicted to it. The addiction broke up his marriage and hurt his family. He knew he would not survive the environment he had found himself in. He was very emotional during the entire assessment. Though he had to wait two days, he was finally sent to detox and then treatment. He decided on his own that it was not in his best interest to return to Wilson. After treatment, he went into a recovery home out of town. He got a job and walked to work to a fast food place. Eventually he bought a bicycle. He continued support groups and put in the work it takes to be free of addiction. He is now reconciled with his children and parents.
Another time, a grandparent brought in his grandson who was using heroin. The grandson was not working and the wife was using too. They had a young child together who was growing up in that environment. The grandson went to detox, came out and returned to use. (Treatment doesn’t work until the client wants it to work.) He found himself in and out of jail for several years. Later, he learned how much trauma he was suffering from as the result of his mother dying early in his life. He returned to treatment on his own. He cleared his outstanding warrants and court dates and is now holding down a job.
|
For more information: Terry Pierce Hope Alliance Coordinator Victim Assistance Wilson Police Department 120 Goldsboro Street Wilson North Carolina 27894 252-399-2352 [email protected] |
Wilson Professional Services Opioid Treatment Provider (WPS/BHG)
WPS is an Outpatient Medicated Assisted Treatment for Opioid Use Disorder. We offer treatment that is usually stigmatized by the public. At WPS, clients have a safe place to receive services and have the opportunity to live a normal life.
WPS is a daily dosing facility. Though WPS only treats opioid use disorders, we screen for several other substances as well. We provide medication-assisted treatment, combined with counseling and group therapy (psychosocial treatment of the disease), to help opiate addicted individuals refrain from using narcotics. We take a holistic approach by treating the addiction and the whole person. To ensure the highest level of care and provide for the best outcomes, we provide treatment planning tailored to each individual patient. Clients must meet certain criteria to take meds out of the facility. Clients start coming in as early as 6 a.m. because of clients holding jobs.
One thing WPS would like the public to know and accept is that addiction does not discriminate. It can happen to anyone regardless of poverty, education, social status, no matter who you are or where you come from. Everyone is affected by addiction, somehow, some way. We are willing to travel to your location and educate you about reducing the stigma of addiction and teach you to use Narcan (naloxone) to save lives. Education and Narcan kits are free to the public.
There are several ways a client is referred to treatment at WPS:
• Word of mouth
• Court ordered
• Outside providers
• Walk ins
We have many success stories we can share. However, one of our favorites is about a patient we were treating for opioid use disorder who became pregnant while in treatment. Because of our services and her faithfulness to stay the course of her treatment, she maintained her sobriety and was able to keep custody of her child.
WPS is an Outpatient Medicated Assisted Treatment for Opioid Use Disorder. We offer treatment that is usually stigmatized by the public. At WPS, clients have a safe place to receive services and have the opportunity to live a normal life.
WPS is a daily dosing facility. Though WPS only treats opioid use disorders, we screen for several other substances as well. We provide medication-assisted treatment, combined with counseling and group therapy (psychosocial treatment of the disease), to help opiate addicted individuals refrain from using narcotics. We take a holistic approach by treating the addiction and the whole person. To ensure the highest level of care and provide for the best outcomes, we provide treatment planning tailored to each individual patient. Clients must meet certain criteria to take meds out of the facility. Clients start coming in as early as 6 a.m. because of clients holding jobs.
One thing WPS would like the public to know and accept is that addiction does not discriminate. It can happen to anyone regardless of poverty, education, social status, no matter who you are or where you come from. Everyone is affected by addiction, somehow, some way. We are willing to travel to your location and educate you about reducing the stigma of addiction and teach you to use Narcan (naloxone) to save lives. Education and Narcan kits are free to the public.
There are several ways a client is referred to treatment at WPS:
• Word of mouth
• Court ordered
• Outside providers
• Walk ins
We have many success stories we can share. However, one of our favorites is about a patient we were treating for opioid use disorder who became pregnant while in treatment. Because of our services and her faithfulness to stay the course of her treatment, she maintained her sobriety and was able to keep custody of her child.
|
Amber Leclercq, CADC
Program Director BHG Wilson Professional Services Treatment Center 3709 Nash Street NW Wilson, NC 27896 O: 252-206-5799 / F: 252-206-5778 Visit bhgrecovery.com |
Opioid Prevalence and MAT (Medication-Assisted Treatment) Data
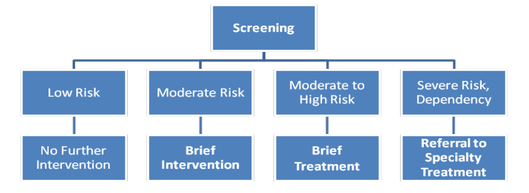
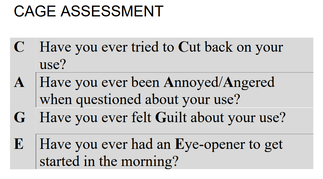
The SBIRT Process (Screening, Brief Intervention & Referral to Treatment)
SBIRT is an exciting way to change and impact how we address substance use and transform the way we partner with people in our community around substance use concerns. SBIRT is an opportunity to start the change in how we think and therefore address substance use. SBIRT provides us, the community, the skills, knowledge, and confidence to build our community competency and capacity to identify, address and talk about substance use. SBIRT takes substance use out of the shadows and hidden corners into the light of healing.
One of my favorite things about SBIRT is that you do not need a special license or credential to do it. Best practice is to take evidenced based training to become familiar with how to utilize evidenced based screening tools (S) , techniques for brief interventions (BIs) and conduct referrals to treatment (RTs). Also, most evidenced based screening tools are free, do not require any credentials or license, and can be self-administered. Here is a handy list: https://www.drugabuse.gov/nidamed-medical-health-professionals/screening-tools-resources/chart-screening-tools
SBIRT is an exciting way to change and impact how we address substance use and transform the way we partner with people in our community around substance use concerns. SBIRT is an opportunity to start the change in how we think and therefore address substance use. SBIRT provides us, the community, the skills, knowledge, and confidence to build our community competency and capacity to identify, address and talk about substance use. SBIRT takes substance use out of the shadows and hidden corners into the light of healing.
One of my favorite things about SBIRT is that you do not need a special license or credential to do it. Best practice is to take evidenced based training to become familiar with how to utilize evidenced based screening tools (S) , techniques for brief interventions (BIs) and conduct referrals to treatment (RTs). Also, most evidenced based screening tools are free, do not require any credentials or license, and can be self-administered. Here is a handy list: https://www.drugabuse.gov/nidamed-medical-health-professionals/screening-tools-resources/chart-screening-tools
It's important that the trainer follow their professional judgment that they are fully competent in all aspects of SBIRT. It also helps to have clinical experience doing SBIRT, a strong knowledge of motivational interviewing and substance use disorders. A second component that is also important is understanding implementation science to help support successful organizational implementation of SBIRT. It's not enough to just know how to perform SBIRT, it's also critical that the trainer provides support in how an organization plans to successfully implement and sustain SBIRT and becomes part of the organizational culture.
I have been very fortunate in my career to have worked nationally with a wide range of providers and organizations. Empowering primary care providers, licensed behavioral health clinicians, care managers, peer recovery coaches, and community support teams to feel confident and competent to start to address substance use disorders is helping to change the way our communities treat people. All our people! SBIRT helps bring compassion, understanding, and support back into the spirit of the work that we do in the heartfelt way we set out from. So SBIRT is not only supporting people around substance use, it's also a way to reinvigorate the healthcare workforce.
I have been very fortunate in my career to have worked nationally with a wide range of providers and organizations. Empowering primary care providers, licensed behavioral health clinicians, care managers, peer recovery coaches, and community support teams to feel confident and competent to start to address substance use disorders is helping to change the way our communities treat people. All our people! SBIRT helps bring compassion, understanding, and support back into the spirit of the work that we do in the heartfelt way we set out from. So SBIRT is not only supporting people around substance use, it's also a way to reinvigorate the healthcare workforce.
|
Nick Szubiak, MSW, LCSW
Principal, NSI Strategies (808) 895.7679 www.nsistrategies.com twitter.com/nszubiak linkedin.com/in/nick-szubiak |
EASTPOINTE Behavioral Health Managed Care Organization
Eastpointe plays a vital role in the communities we serve. We help our most vulnerable residents find quality behavioral healthcare when and where they need it. We are on the ground, every day, strengthening communities by providing behavioral health education and making investments in projects and organizations that help improve residents' quality of life. Many of our employees live in our service area and have been helping provide for their neighbors' behavioral health needs for decades.
Eastpointe works together with individuals, families, providers, and communities to achieve valued outcomes in our behavioral healthcare system.
Eastpointe is a Managed Care Organization (MCO) dedicated to working with individuals and families in eastern North Carolina who struggle with substance use, mental health, and intellectual and developmental disabilities. In partnership with community agencies, licensed independent practitioners and hospitals, we help the uninsured and those with Medicaid get comprehensive, effective treatment that is essential for their well-being.
Eastpointe is a Managed Care Organization, so we are not legally allowed to provide direct services like the historic Mental Health Centers. As a MCO we are responsible for managing, coordinating, facilitating, and monitoring the provision of state, federal, and Medicaid funded mental health, intellectual and developmental disability, and substance use services for members in the Eastpointe catchment area (Duplin, Edgecombe, Greene, Lenoir, Robeson, Sampson, Scotland, Warren, Wayne, and Wilson Counties.)
• Functions of the MCO are:
• 24/7/365 Access to Care (connects individuals to treatment, crisis services, or community resources)
• Review of Service Authorization Requests
• Care Coordination
• Provider Network Development/Monitoring
• Grievance and Appeals
• Quality Improvement (Data Driven)
• Other Business Operations (IT, HR, Finance, etc)
• Claims Processing/Provider Payment
• Education/Prevention/Outreach
Our member call center is available 24/7/365 by calling 1-800-913-6109. Anyone in need of services is encouraged to call and our staff will connect them with the most appropriate services or resources.
Eastpointe plays a vital role in the communities we serve. We help our most vulnerable residents find quality behavioral healthcare when and where they need it. We are on the ground, every day, strengthening communities by providing behavioral health education and making investments in projects and organizations that help improve residents' quality of life. Many of our employees live in our service area and have been helping provide for their neighbors' behavioral health needs for decades.
Eastpointe works together with individuals, families, providers, and communities to achieve valued outcomes in our behavioral healthcare system.
Eastpointe is a Managed Care Organization (MCO) dedicated to working with individuals and families in eastern North Carolina who struggle with substance use, mental health, and intellectual and developmental disabilities. In partnership with community agencies, licensed independent practitioners and hospitals, we help the uninsured and those with Medicaid get comprehensive, effective treatment that is essential for their well-being.
Eastpointe is a Managed Care Organization, so we are not legally allowed to provide direct services like the historic Mental Health Centers. As a MCO we are responsible for managing, coordinating, facilitating, and monitoring the provision of state, federal, and Medicaid funded mental health, intellectual and developmental disability, and substance use services for members in the Eastpointe catchment area (Duplin, Edgecombe, Greene, Lenoir, Robeson, Sampson, Scotland, Warren, Wayne, and Wilson Counties.)
• Functions of the MCO are:
• 24/7/365 Access to Care (connects individuals to treatment, crisis services, or community resources)
• Review of Service Authorization Requests
• Care Coordination
• Provider Network Development/Monitoring
• Grievance and Appeals
• Quality Improvement (Data Driven)
• Other Business Operations (IT, HR, Finance, etc)
• Claims Processing/Provider Payment
• Education/Prevention/Outreach
Our member call center is available 24/7/365 by calling 1-800-913-6109. Anyone in need of services is encouraged to call and our staff will connect them with the most appropriate services or resources.
|
Community Inclusion Member Story
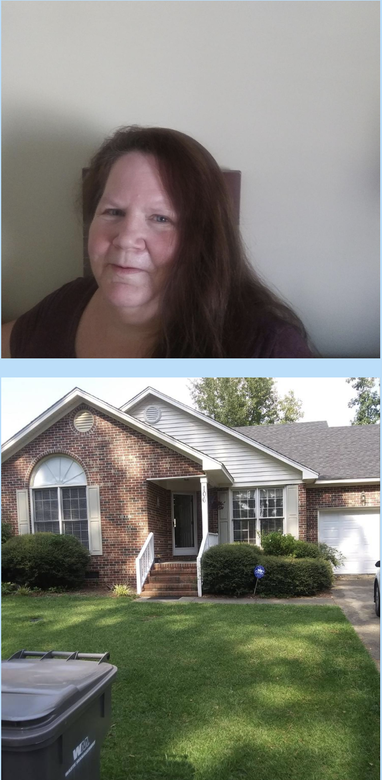
Patricia “Pattie” Lee entered the The Transitions to Community Living Initiative (TCLI) program in 2018. Eastpointe learned of her interest in TCLI during an outreach visit to the Hamlet House Adult Care Home, where she was recovering from medical problems, ending her cocaine addiction and working through her diagnosis of Major Depressive Disorder. Pattie moved into a two-bedroom, two-bathroom house with a front porch and a garage on August 30, 2018. The property also has a big backyard so she can play with her seven grandchildren. Because of limited transportation options and her fixed income, Eastpointe referred Pattie to Alliance of Disability Advocates of North Carolina (ADANC) to participate in the Community Inclusion program. Her Community Inclusion Specialist from ADANC assisted her with creating a community engagement plan and setting goals. As part of the plan, ADANC assisted her with getting a certified emotional support dog named Lucky. Pattie has been determined to execute her plan. She’s now actively involved with her church activities at the Jehovah Witness Kingdom Hall. She’s devoted to “Jehovah” for giving her the spiritual guidance to maintain her sobriety. She has maintained her sobriety for what will have been three years in January 2020. Given all she has to look forward to, Pattie plans to stay that way. She gives all praise to Eastpointe’s TCLI Program, ADANC, and Jehovah for her success in her beautiful home. |
|
This is the link to our 2021 Annual Report, which is posted on our website and may provide additional helpful information:
https://mco.eastpointe.net/DocumentBrowser/Media-Library/EP2021AnnualReportDigital.pdf |
(Client’s name, photo and story have been shared with written and signed permission.)
|
Carolina Family Health Center (CFHC)
Carolina Family Health Centers holds a vital role in our community – both as a quality resource for health care and a trusted community partner.
As a health care resource, CFHC provides comprehensive, culturally competent and cost effective primary and preventative care. As a federally qualified community health center, our doors are open to all members of the community, regardless of health insurance status or ability to pay. Our goal is to eliminate as many barriers to care as possible to ensure healthcare is accessible to all community members.
CFHC’s Medication Assisted Treatment (MAT) program was started in June 2019 at Freedom Hill Community Health Center in Tarboro, expanded to Wilson Community Health Center in 2020, and will be expanding to Harvest Family Health Center in Elm City in the very near future. The MAT program is offered for alcohol and opioid use disorders. This program is important for our community because it opens access to treatment options with a link to other healthcare services to improve overall health and wellbeing.
Partnerships are key to strong healthy communities. CFHC has relationships with many agencies and organizations which allows us to access external services for our patients and to be a resource for the clients and customers of our partners. Through collaborations, CFHC and its partners are able to identify the needs of the community and devise creative strategies using the strengths of each partner to address the needs.
Carolina Family Health Centers has a mission to provide accessible and affordable health care with excellence…where patients come first. Our vision is to be a trusted resource for patients, to address as many health needs as possible under one roof, to eliminate barriers that often prevent individuals from getting the care they need, and to educate and engage patients in their healthcare.
CFHC’s services are available to anyone and everyone. A core component of our health care model is to reach medically underserved and rural areas and care for vulnerable populations. For individuals without insurance, we offer a sliding scale discount program to adjust fees based on household income and size.
Specific to MAT treatment, a behavioral health clinician performs an initial assessment before a provider visit is scheduled to determine eligibility/good fit for our program. If a patient is not a good candidate for us, then they are referred to a different program. At each visit, the patient first sees the clinician for a brief therapy session, then sees the medical provider, who addresses as many simultaneous health care needs as time permits to decrease the number of visits. The treatment plan is individualized to fit the patient, and the goal is to incorporate substance use treatment seamlessly into primary care services.
Research shows that a combination of medication and therapy can successfully treat substance use disorders, and for some people struggling with addiction, MAT can help sustain recovery. MAT is also used to prevent or reduce opioid overdose. The goals of CFHC’s MAT program are to promote long-term recovery and reduce the potential for overdose for patients who struggle with opiate, opioid and alcohol use disorders in our community.
CFHC provides medical, behavioral health, pharmacy and dental services. CFHC operates three medical facilities with in-house pharmacies and one dental facility across Wilson, Nash and Edgecombe counties.
• Medical services include adult medicine, pediatrics, physical exams, immunizations, gynecology and HIV/AIDS care.
• Pharmacy services include dispensing services at each medical location, medication adherence services, Medicare Part D counseling and medication delivery.
• Dental services include dental exams, teeth cleaning, oral cancer screenings, filings, crowns and bridges, tooth extractions and dentures.
• Behavioral health services include one-on-one counseling, grief and loss therapy, depression and anxiety screening and counseling and substance use treatment. CFHC provides a fully integrated primary care/behavioral health model of care with a Licensed Clinical Social Worker (LCSW) on-site at each delivery location for behavioral health services. The Integrated Behavioral Health (IBH) team provides individual behavioral health and substance use counseling.
• Additional enabling services include transportation assistance, language assistance, migrant farmworker outreach, diabetes education and counseling, insurance enrollment assistance, and specialty referrals.
• Specific to MAT
▪ MAT programs are offered for alcohol and opioid use disorders in a team based care model that combines primary care, MAT, and behavioral health counseling all together in one visit. MAT providers also treat hepatitis C and sexually transmitted infections. The program offers low threshold buprenorphine induction and dispensing syringes from each of its pharmacies for MAT patients who inject drugs. Nasal naloxone is given free of charge to all patients when they start the program, and refilled based on need. The program has a particular focus on the use of long acting injectable buprenorphine (Sublocade®), since this option allows for more comprehensive medication coverage and decreases issues with compliance. MAT patients have access to discounted medication from our in-house pharmacies and drug manufacturer patient assistance programs and savings cards.
▪ CFHC’s MAT program operates from a harm reduction philosophy with a focus on keeping patients engaged and accountable, while reinstating structure and responsibilities with time. Treatment plans are individualized for every patient, recognizing that there is no “one size fits all” success plan.
▪ 38 patients have received MAT for OUD since the start of this service (2/22/2021) at WCHC
▪ 37 patients have received MAT for AUD since the start of this service (6/19/2020) at WCHC
For primary care, IBH and dental services, individuals can call any of our centers to schedule an appointment.
For MAT services, individuals can call (252) 641-0514, Extension 410 to speak with a behavioral health clinician and schedule an appointment.
One of the most remarkable successes we've had is with a patient who had used heroin and fentanyl on a daily basis for over 30 years. He had been to several treatment centers and inpatient detoxification in the past, but continued to return to use despite treatment. He knew he was at significant risk of overdose and came to us for help. He had a rough start transitioning to medication initially, with underlying medical issues that made treatment more complicated, but with perseverance he was able to transition to oral medication. He was then able to change to a once monthly injection of buprenorphine, which has been an extremely effective approach. It has been over a year since he used heroin or fentanyl, and he tells us at every visit that this treatment plan saved his life.
Carolina Family Health Centers holds a vital role in our community – both as a quality resource for health care and a trusted community partner.
As a health care resource, CFHC provides comprehensive, culturally competent and cost effective primary and preventative care. As a federally qualified community health center, our doors are open to all members of the community, regardless of health insurance status or ability to pay. Our goal is to eliminate as many barriers to care as possible to ensure healthcare is accessible to all community members.
CFHC’s Medication Assisted Treatment (MAT) program was started in June 2019 at Freedom Hill Community Health Center in Tarboro, expanded to Wilson Community Health Center in 2020, and will be expanding to Harvest Family Health Center in Elm City in the very near future. The MAT program is offered for alcohol and opioid use disorders. This program is important for our community because it opens access to treatment options with a link to other healthcare services to improve overall health and wellbeing.
Partnerships are key to strong healthy communities. CFHC has relationships with many agencies and organizations which allows us to access external services for our patients and to be a resource for the clients and customers of our partners. Through collaborations, CFHC and its partners are able to identify the needs of the community and devise creative strategies using the strengths of each partner to address the needs.
Carolina Family Health Centers has a mission to provide accessible and affordable health care with excellence…where patients come first. Our vision is to be a trusted resource for patients, to address as many health needs as possible under one roof, to eliminate barriers that often prevent individuals from getting the care they need, and to educate and engage patients in their healthcare.
CFHC’s services are available to anyone and everyone. A core component of our health care model is to reach medically underserved and rural areas and care for vulnerable populations. For individuals without insurance, we offer a sliding scale discount program to adjust fees based on household income and size.
Specific to MAT treatment, a behavioral health clinician performs an initial assessment before a provider visit is scheduled to determine eligibility/good fit for our program. If a patient is not a good candidate for us, then they are referred to a different program. At each visit, the patient first sees the clinician for a brief therapy session, then sees the medical provider, who addresses as many simultaneous health care needs as time permits to decrease the number of visits. The treatment plan is individualized to fit the patient, and the goal is to incorporate substance use treatment seamlessly into primary care services.
Research shows that a combination of medication and therapy can successfully treat substance use disorders, and for some people struggling with addiction, MAT can help sustain recovery. MAT is also used to prevent or reduce opioid overdose. The goals of CFHC’s MAT program are to promote long-term recovery and reduce the potential for overdose for patients who struggle with opiate, opioid and alcohol use disorders in our community.
CFHC provides medical, behavioral health, pharmacy and dental services. CFHC operates three medical facilities with in-house pharmacies and one dental facility across Wilson, Nash and Edgecombe counties.
• Medical services include adult medicine, pediatrics, physical exams, immunizations, gynecology and HIV/AIDS care.
• Pharmacy services include dispensing services at each medical location, medication adherence services, Medicare Part D counseling and medication delivery.
• Dental services include dental exams, teeth cleaning, oral cancer screenings, filings, crowns and bridges, tooth extractions and dentures.
• Behavioral health services include one-on-one counseling, grief and loss therapy, depression and anxiety screening and counseling and substance use treatment. CFHC provides a fully integrated primary care/behavioral health model of care with a Licensed Clinical Social Worker (LCSW) on-site at each delivery location for behavioral health services. The Integrated Behavioral Health (IBH) team provides individual behavioral health and substance use counseling.
• Additional enabling services include transportation assistance, language assistance, migrant farmworker outreach, diabetes education and counseling, insurance enrollment assistance, and specialty referrals.
• Specific to MAT
▪ MAT programs are offered for alcohol and opioid use disorders in a team based care model that combines primary care, MAT, and behavioral health counseling all together in one visit. MAT providers also treat hepatitis C and sexually transmitted infections. The program offers low threshold buprenorphine induction and dispensing syringes from each of its pharmacies for MAT patients who inject drugs. Nasal naloxone is given free of charge to all patients when they start the program, and refilled based on need. The program has a particular focus on the use of long acting injectable buprenorphine (Sublocade®), since this option allows for more comprehensive medication coverage and decreases issues with compliance. MAT patients have access to discounted medication from our in-house pharmacies and drug manufacturer patient assistance programs and savings cards.
▪ CFHC’s MAT program operates from a harm reduction philosophy with a focus on keeping patients engaged and accountable, while reinstating structure and responsibilities with time. Treatment plans are individualized for every patient, recognizing that there is no “one size fits all” success plan.
▪ 38 patients have received MAT for OUD since the start of this service (2/22/2021) at WCHC
▪ 37 patients have received MAT for AUD since the start of this service (6/19/2020) at WCHC
For primary care, IBH and dental services, individuals can call any of our centers to schedule an appointment.
For MAT services, individuals can call (252) 641-0514, Extension 410 to speak with a behavioral health clinician and schedule an appointment.
One of the most remarkable successes we've had is with a patient who had used heroin and fentanyl on a daily basis for over 30 years. He had been to several treatment centers and inpatient detoxification in the past, but continued to return to use despite treatment. He knew he was at significant risk of overdose and came to us for help. He had a rough start transitioning to medication initially, with underlying medical issues that made treatment more complicated, but with perseverance he was able to transition to oral medication. He was then able to change to a once monthly injection of buprenorphine, which has been an extremely effective approach. It has been over a year since he used heroin or fentanyl, and he tells us at every visit that this treatment plan saved his life.